Comparison of marginal and internal fit of zirconia crowns fabricated by three-dimensional printing with different offset parameters: A preliminary pilot study
Article information
Abstract
Purpose
This study aimed to evaluate the marginal and internal fit of zirconia crowns fabricated using 3-dimensional (3D) printing technology with different offset parameters.
Materials and Methods
A maxillary right first molar of a standard typodont (D85DP-500B.1; Nissin Dental, Kyoto, Japan) was prepared for a zirconia crown with a 1.0 mm margin. Virtual casts were obtained using an intraoral scanner (i700; MEDIT, Seoul, Republic of Korea). Crown designs were created with CAD software (Dentbird; IMAGOWORKS, Seoul, Republic of Korea) using specific parameters: cement space (50 µm), adaptive extra gap (0 µm), height for minimal gap (50 µm), and margin width (100 µm). Zirconia crowns were fabricated using a vat photopolymerization DLP 3D printer (TD6+; 3D Controls, Busan, Republic of Korea). Two offset groups were defined: the Offset -70 µm group (outermost XY-direction pixels reduced by one unit) and the Offset 0 µm group (no adjustment). All crowns were printed with a 50 µm Z-layer thickness. Eighteen crowns were fabricated (N = 9 per group). Marginal and internal fit measurements were conducted using the triple-scan method. The measured marginal and internal gaps were statistically compared using an independent t-test (α = 0.05).
Results
The offset -70 µm group demonstrated significantly smaller marginal gaps (P<0.05) and internal gaps (P>0.05) compared to the offset 0 µm group.
Conclusion
These findings suggest that adjusting the XY-direction offset may help minimize manufacturing errors, enhancing the overall accuracy of zirconia crown fabrication.
Introduction
The advancement of digital technology has significantly transformed the fabrication of dental prostheses, introducing innovative approaches that enhance efficiency, precision, and clinical predictability [1–3]. Among these advancements, three-dimensional (3D) printing has emerged as a disruptive technology in prosthodontics, integrating digital design with additive manufacturing to enable highly customized restorations with improved accuracy [4,5]. Initially limited to polymer-based materials, 3D printing has evolved to include ceramics such as zirconia, a biocompatible material with excellent mechanical strength, wear resistance, and esthetic properties [6–8]. This progress has expanded the clinical applicability of 3D printing, particularly in the fabrication of fixed dental prostheses [9,10].
Compared to subtractive manufacturing techniques such as milling, 3D printing offers several advantages, including reduced material waste, the elimination of tool wear, and enhanced cost efficiency [11–13]. Zirconia is widely used in fixed prosthodontics due to its superior mechanical properties, chemical stability, and esthetics [14,15]. however, fabricating zirconia restorations via 3D printing presents inherent challenges. post-processing steps such as debinding and sintering are time-intensive and can introduce dimensional inaccuracies, potentially compromising the final restoration's fit [16,17]. Given the stringent precision requirements in fixed prosthodontics, even minor deviations can negatively impact clinical outcomes [18–20].
The long-term success of fixed dental prostheses is largely dependent on their marginal and internal fit [20–22]. Marginal fit refers to the adaptation of the restoration’s margin to the prepared tooth structure and is critical for preventing plaque accumulation, maintaining periodontal health, and ensuring restoration longevity [23,24]. Poor marginal adaptation is associated with increased risks of secondary caries, periodontal inflammation, and prosthetic failure [25]. Internal fit pertains to the uniformity of the cement space between the restoration and the prepared tooth surface, which directly affects retention, stability, and durability [26]. Inadequate internal adaptation may result in uneven cement distribution, reduced bonding strength, and an increased likelihood of prosthesis dislodgment [27,28]. therefore, optimizing both marginal and internal fit is essential for achieving predictable and durable clinical outcomes.
Digital Light Processing (DLP) is a widely utilized 3D printing technique in prosthetic dentistry due to its ability to produce high-resolution restorations with fine detail reproduction [29-31]. This technology employs a digital micromirror device to project pixel-level images, enabling precise layer-by-layer polymerization of ceramic suspensions [32]. a unique advantage of DLP-based 3D printing is the ability to apply XY-direction offset adjustments during the fabrication process to compensate for potential inaccuracies introduced during printing and post-processing [33,34]. this feature is particularly beneficial for zirconia restorations, as it can improve the final prosthesis's dimensional accuracy and fit.
Despite the advantages of pixel-level adjustments, limited research has investigated the impact of offset parameters on the marginal and internal fit of zirconia crowns fabricated using DLP 3D printing. the offset parameter plays a crucial role in defining crown dimensions and adaptation accuracy, yet there is a lack of standardized guidelines for optimal offset values. therefore, the purpose of this study aims to address this gap by evaluating the effect of two offset settings, -70 μm and 0 μm, on the marginal and internal fit of zirconia crowns fabricated with DLP 3D printing. In the offset -70 μm group, the outermost pixels in the XY direction were reduced by one unit (-70 μm) to minimize dimensional discrepancies, whereas in the offset 0 μm group, no pixel adjustment was applied. this study hypothesizes that applying a -70 μm offset will result in a significantly improved marginal and internal fit compared to no offset adjustment. the null hypothesis assumes no significant difference in the fit between the two groups. by analyzing the impact of pixel offset adjustments, this study seeks to contribute to the optimization of zirconia 3D printing processes and provide clinically relevant insights for enhancing the accuracy and predictability of additively manufactured zirconia restorations.
Materials and Methods
1. Sample preparation
This study was designed as a preliminary pilot study to evaluate the effect of offset parameters on the marginal and internal fit of zirconia crowns fabricated using DLP 3D printing. The sample size calculation was performed using a power software (G*Power 3.1.9.7; Heinrich-Heine-University, Düsseldorf, Germany) to achieve a statistical power of 80% (1-β = 0.80) with an effect size (d) of 1.5 and an alpha level (α) of 0.05. Based on this calculation, a minimum of eight specimens per group was required. To account for potential variability in fabrication and measurement processes, a total of nine specimens were allocated per group (N = 9), providing a balance between statistical robustness and practical feasibility.
Tooth preparation was performed on the maxillary right first molar of a standard typodont model (D85DP-500B.1; Nissin Dental, Tokyo, Japan), and the crown was designed accordingly. the maxillary right first molar was prepared with a chamfer-shaped finish line, ensuring a smooth transition for the restoration. the axial walls were reduced by 1.0 mm, while the occlusal surface was reduced by 1.5 mm to provide sufficient space for the zirconia crown. The finish line was positioned supragingivally to facilitate precise scanning and margin adaptation.
To obtain a virtual cast, the maxillary right first molar and adjacent teeth were scanned using an intraoral scanner (i700; MEDIT, Seoul, Republic of Korea). The opposing teeth and occlusal record scans were also acquired to ensure proper occlusal alignment.
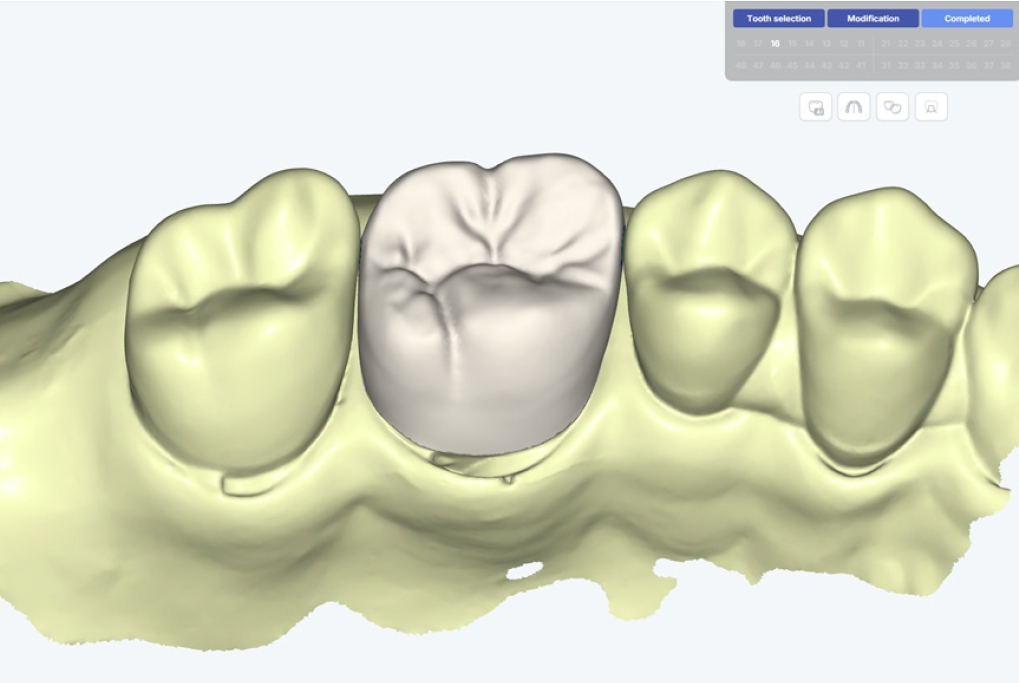
The crown design was performed using CAD software (Dentbird; IMAGOWORKS, Seoul, Korea), specifically configured for zirconia crowns (Fig. 1). The cement space was set to 50 μm, and the crown morphology was generated using an AI-based design feature. The design parameters were as follows: cement space: 50 μm; adaptive extra gap: 0 μm; height for minimal gap: 50 μm; margin width: 100 μm. to designate the marginal region of the crown, the area extending 1.0 mm from the finish line of the tooth preparation was set with a cement space of 0 μm. The generated morphology was verified by an experienced professional with expertise in digital crown design.
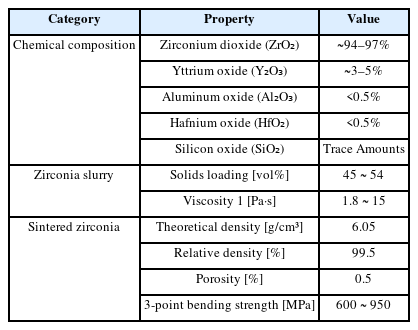
The crowns were fabricated using zirconia material (3DCERA; 3D Controls, Busan, Korea) and a vat photopolymerization DLP 3D printer (TD6+; 3D Controls, Busan, Korea) (Table 1, Fig. 2). The slicing software (3D Controls Slicer; 3D Controls, Busan, Korea) was used to process the printing data.
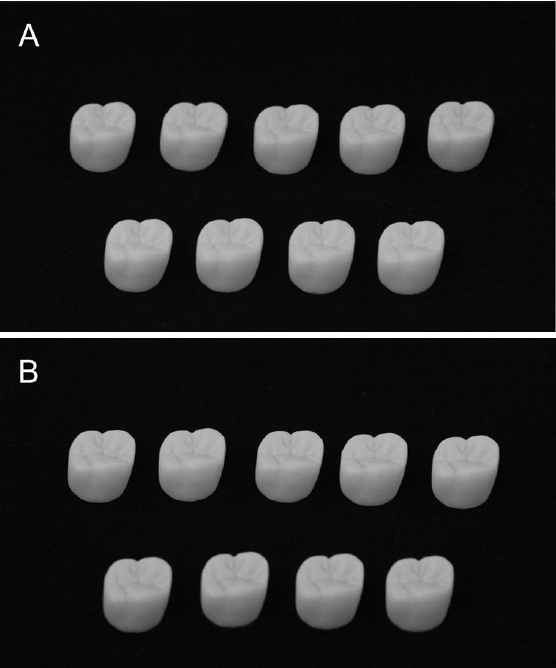
Zirconia crowns fabricated using two different 3D printing parameters. A. Crown fabricated with the offset 0 μm parameter. B. Crown fabricated with the offset -70 μm parameter.
The 3D printer (TD6+; 3D Controls, Busan, Korea) used in this study had a pixel size of 70 μm in the XY direction, and the detailed composition of the zirconia material is presented in Table 1. Two offset parameter groups were established: the Offset -70 μm group, in which the outermost pixels in the XY direction were reduced by one unit (-70 μm) to compensate for potential printing inaccuracies, and the Offset 0 μm group, where no pixel adjustments were applied. given that a pixel size of the 3D printer was 70 μm, the -70 μm offset parameter was determined based on this resolution to enhance dimensional accuracy. The build orientation of the crowns was standardized, and the layer thickness in the Z-direction was set to 50 μm. A total of 18 crowns were fabricated (N = 9 per group), and following printing, the crowns underwent post-processing procedures, including cleaning, debinding, and sintering, to ensure proper specimen preparation.
2. Marginal and internal fit
The marginal and internal fit of the crowns was evaluated using a triple-scan protocol, as follows: 1) scan data 1: The intaglio and occlusal surfaces of the crown were scanned using a laboratory scanner (E1; 3Shape, Copenhagen, Denmark); 2) Scan data 2: The typodont model (D85DP-500B.1; Nissin Dental, Tokyo, Japan) was scanned using the same laboratory scanner; 3) scan data 3: The crown was seated onto the typodont model, and this assembly was scanned to acquire the final dataset. the crown adaptation process was supervised by an experienced operator, ensuring that the crown was properly seated on the typodont model before scanning.
The acquired scan data were processed and aligned using 3D inspection software (Geomagic Control X; 3D Systems, Rock Hill, SC, USA). the alignment procedure involved initial registration, followed by best-fit alignment, with scan data 3 serving as the reference for aligning scan data 1 and scan data 2 (Fig. 3).
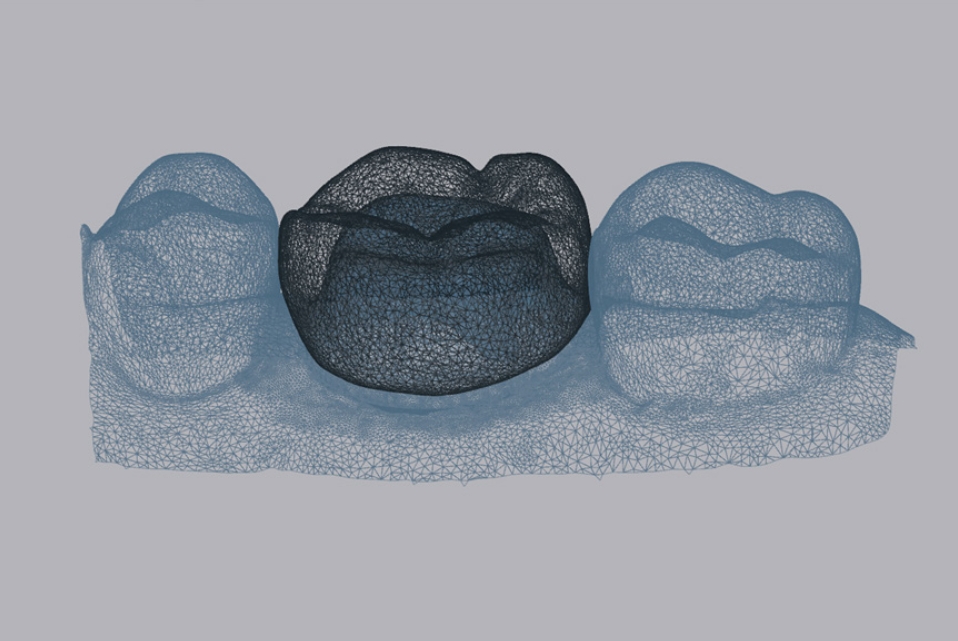
Alignment of crown and typodont model scan data. The scan data obtained from the crown (black color) and typodont model (blue color) were aligned using 3D inspection software to evaluate marginal and internal fit.
The marginal and internal gaps were quantified using the root mean square (RMS) of the mean distances between the crown's intaglio surface mesh and the tooth preparation surface mesh of the typodont model, using 3D inspection software (Geomagic Control X; 3D Systems, Rock Hill, SC, USA). the RMS value was calculated using the following equation:
where X1,i represents the i-th measurement point on the intaglio surface mesh of the crown, and X2,i represents the corresponding measurement point on the tooth preparation surface mesh of the typodont model. The RMS value quantifies the mean absolute distance between these two mesh surfaces, thereby serving as an indicator of the marginal and internal gaps. thus, the RMS value reflects the discrepancy between the crown’s intaglio surface and the corresponding points on the tooth preparation surface, effectively representing the marginal and internal fit. The results were visualized as a color map, with the range set to ±500 μm, where the green zone denoted an acceptable tolerance of 100 μm.
To assess the marginal and internal fit of the fabricated zirconia crowns, the marginal gap and internal gap were measured. according to previous literature, including the widely referenced study by Holmes et al. [35], the marginal gap is defined as the perpendicular distance between the finish line of the tooth preparation and the crown margin, encompassing any discrepancies at the margin. the internal gap refers to the space between the intaglio surface of the crown and the prepared tooth surface, which includes the axial and occlusal discrepancies. in this study, 3D analysis was conducted, and the measurement regions were designated following established methodologies [36]. The marginal region was defined as the area extending 1.0 mm above the finish line of the tooth preparation, where no cement space was assigned. The entire 1.0 mm width of the prepared margin was considered part of the marginal gap measurement, ensuring that any discrepancies at the crown margin were accounted for. the internal gap was assessed in the region superior to the marginal region, encompassing the axial and occlusal surfaces of the preparation. specifically, the axial internal gap was measured in the vertical plane along the axial walls, while the occlusal internal gap was measured at the central and cusp tip areas of the occlusal surface. these definitions were applied to enhance clarity and consistency in interpreting the results.
3. Statistical analysis
All data for the marginal and internal fit of the crowns fabricated under the two parameter conditions (offset -70 μm group and offset 0 μm group) were analyzed using statistical software (IBM SPSS Statistics v25.0; IBM Corp, Armonk, NY, USA) with a significance level set at α = 0.05. To assess the normality of the data, the shapiro-wilk test was performed, confirming that the data followed a normal distribution. to compare the results between the two parameter conditions, an independent t-test was used to evaluate the statistical significance between the two groups.
Results
the marginal and internal fit values of zirconia crowns fabricated under the two different offset conditions are summarized in Table 2. The mean marginal gap was significantly smaller in the offset -70 μm group (77.6 ± 9.7 μm) than in the offset 0 μm group (97.0 ± 9.8 μm, P<0.05). The mean internal gap was also significantly smaller in the offset -70 μm group (90.4 ± 10.3 μm) compared to the offset 0 μm group (121.2 ± 20.5 μm, P < 0.05). The overall fit followed the same trend, with a significantly reduced gap in the offset -70 μm group (91.4 ± 10.0 μm) compared to the offset 0 μm group (121.3 ± 20.1 μm, P < 0.05).
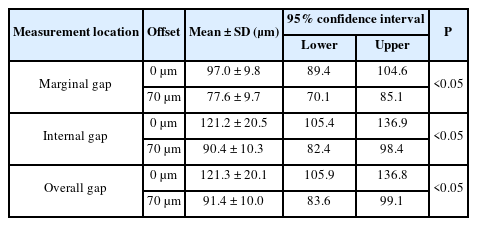
Comparison of the marginal and internal fit of zirconia crowns fabricated by two different 3D printing parameters
Figure 4 provides color difference maps illustrating the marginal and internal fit variations between the two groups. the colors observed in the supragingival region of the abutment indicate the magnitude of the gap, with yellow, orange, and red representing progressively larger discrepancies (Fig. 4). the offset 0 μm group (Figs. 4A, C, and E) displayed a broader distribution of yellow and orange regions, indicating larger discrepancies and reduced fit accuracy. In contrast, the offset -70 μm group (Figs. 4B, D, and F) predominantly exhibited green coloration, demonstrating a closer adaptation within the ±100 μm tolerance range. these visual findings align with the quantitative results, confirming that applying a -70 μm offset significantly improves the marginal and internal fit of zirconia crowns.
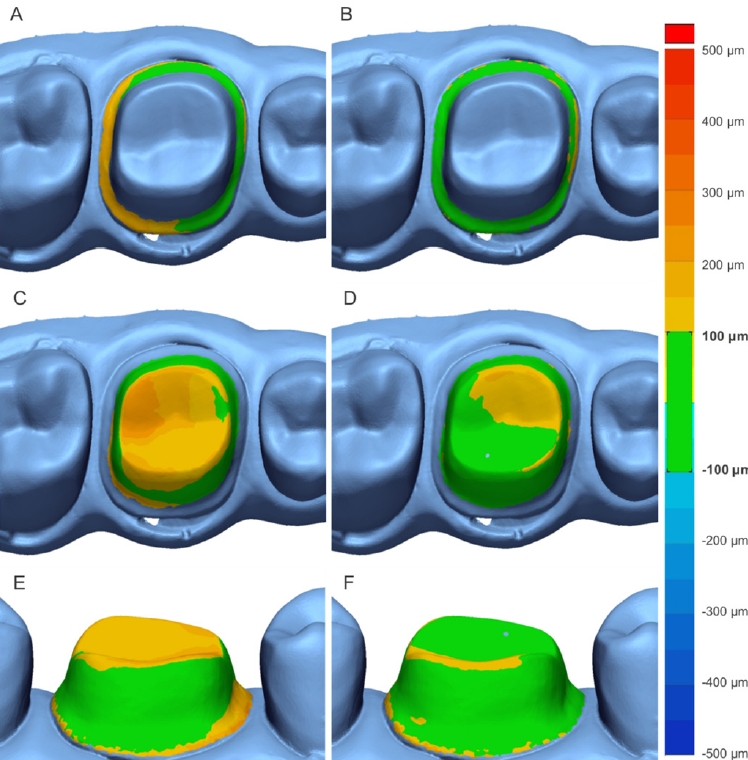
Comparison of color difference maps of the marginal and internal fit of zirconia crowns fabricated by two different 3D printing parameters. A. Marginal gap (offset 0 μm group). B. Marginal gap (offset -70 μm group). C. Internal gap (offset 0 μm group). D. Internal gap (offset -70 μm group). E. Overall gap (offset 0 μm group). F. Overall gap (offset -70 μm group).
Discussion
the null hypothesis stated that there would be no significant difference in the marginal and internal fit of zirconia crowns fabricated with two different offset parameters (-70 μm and 0 μm). however, the results demonstrated that crowns fabricated with the offset -70 μm parameter exhibited significantly smaller marginal (P<0.05) and internal gaps (P<0.05) compared to those fabricated with the offset 0 μm parameter, leading to the rejection of the null hypothesis (P<0.05). these findings suggest that reducing the outermost pixels in the XY direction during the DLP 3D printing process effectively compensates for inaccuracies introduced during printing and post-processing, thereby improving marginal and internal fit. the enhanced fit achieved with the offset -70 μm parameter falls within the clinically acceptable precision threshold of ±100 μm for fixed dental prostheses, indicating its potential to enhance both clinical adaptability and long-term stability of zirconia restorations [20–22,26]. This study highlights the importance of optimizing DLP 3D printing parameters to improve the accuracy and clinical performance of zirconia prostheses, reinforcing the role of digital manufacturing in restorative dentistry [19,33].
Pixel offset adjustments have been identified as an effective method for compensating for inaccuracies in DLP 3D printing, providing precise control over dimensional tolerances at the pixel level. this capability differentiates DLP 3D printing from traditional manufacturing techniques, which lack such fine control and rely on less precise compensatory methods [19,33,34]. previous research has indicated that pixel offset adjustments enhance geometric accuracy in DLP printing [33,34], yet their application in dental restorations, particularly zirconia crowns, has been limited. The findings of this study confirm that implementing a -70 μm pixel offset significantly improves both marginal and internal fit, aligning with established clinical standards. This underscores the necessity of pixel-level adjustments as a key strategy for enhancing the precision and reliability of DLP 3D-printed dental restorations.
while pixel parameter adjustments in DLP 3D printing have been a primary focus in industrial applications, where techniques such as grayscale modulation are employed to refine geometric boundaries [33,34], their adoption in dental prosthetics remains underexplored. this study bridges that gap by demonstrating that a -70 μm pixel offset effectively reduces fabrication discrepancies, leading to superior marginal and internal adaptation in zirconia crowns. these improvements directly influence clinical outcomes, as better marginal adaptation minimizes plaque accumulation and reduces the risk of secondary caries, while enhanced internal fit ensures uniform cement distribution and long-term prosthesis stability [23,26]. the results suggest that pixel-level optimization is not merely a technical adjustment but a clinically relevant modification that enhances the adaptation and longevity of 3D-printed zirconia restorations.
despite the promising potential of zirconia 3D printing in dental applications, several challenges remain unresolved, including prolonged post-processing times, translucency limitations, and material handling complexities [8,16,20,30]. This study contributes by proposing optimized parameters that improve the clinical applicability of zirconia crowns fabricated via DLP 3D printing. however, while pixel offset adjustments improve accuracy, factors such as debinding shrinkage, sintering distortions, and esthetic limitations continue to pose barriers to widespread clinical adoption [14,31]. future advancements should focus on streamlining fabrication workflows to reduce processing times, enhancing zirconia material properties to improve translucency, and developing advanced 3D printing technologies to overcome current limitations. continued innovation in these areas will be critical in maximizing the potential of zirconia 3D printing for restorative applications.
while this study provides meaningful insights into pixel offset adjustments, several limitations should be acknowledged. the small sample size limits the statistical robustness and generalizability of the findings, and future studies should incorporate larger datasets to validate these results. additionally, this study focused exclusively on zirconia crowns, excluding other prosthetic applications; Further research should investigate the impact of pixel adjustments on different materials, including resin and hybrid ceramics, as well as other types of dental prostheses. another limitation is that the study assessed marginal and internal fit immediately after fabrication, without evaluating long-term clinical performance or durability. future studies should include long-term clinical trials assessing prosthesis longevity, cement retention, and biological responses to provide a comprehensive understanding of how pixel offset adjustments influence the accuracy, durability, and functionality of DLP 3D-printed dental restorations.
This study evaluated the effect of pixel offset adjustments on the marginal and internal fit of zirconia crowns fabricated using DLP 3D printing. The results demonstrated that applying a -70 μm offset in the XY direction significantly improved marginal and internal fit compared to the 0 μm offset condition, with all differences reaching statistical significance. these findings indicate that optimizing pixel offset parameters can effectively compensate for manufacturing inaccuracies, enhancing the precision of 3D-printed zirconia restorations.
Thile this study provides valuable insights into parameter optimization in DLP 3D printing, limitations such as the small sample size and lack of long-term clinical validation should be addressed in future research. further studies should explore the impact of offset adjustments on different materials and prosthetic applications, as well as assess the long-term performance of 3D-printed zirconia restorations. optimizing printing parameters remains critical for improving the clinical applicability and reliability of additively manufactured dental prostheses.
Notes
Conflicts of Interest
The zirconia materials used in this research were provided by 3D Controls Co, Ltd. This support had no influence on the study design, data collection, analysis, or interpretation of the results.
Acknowledgment
This research was funded by the Machine Equipment Industry Technology Development (R&D) Program (Project No. RS-2024-00442711) supported by the Ministry of Trade, Industry and Energy (MOTIE, Korea).